With the rising number of deaths from opioids, there is an urgent need to expand the use of Narcan. It has become a vital tool in fighting an epidemic of opioid addiction. In addition, increasing access to this antidote allows bystanders to help with a fatal overdose and save lives.
The CDC reports that more than 932,000 Americans have passed away from drug overdoses since 1999. In 2020, opioids were implicated in about 75% of drug overdose fatalities. Since 1999, the number of overdose deaths involving opioids — including heroin, prescription opioids, and synthetic opioids — has multiplied by more than eightfold.
Likewise, from 2020 onwards, 69,000 individuals died from opioid overdose. Of those, 82% were brought on by synthetic opioids like fentanyl.
So how can we help to avoid some of this tragedy?
In a Utopian society, we would eliminate the existence of opioids outside of medical use. Sadly, as opioid use becomes more frequent in times of isolation and economic uncertainty: this may never be the case.
Realistically, treating opiate overdose as quickly as possible is the best course of action, which is why the use of Narcan right away is so crucial.
Naloxone: An Overdose Reversal Drug
The generic drug Naloxone, also known by the brand name Narcan, was initially given FDA approval in 1971. A vital tool to temporarily reverse the effects of an opioid overdose, Narcan comes as a nasal spray.
Narcan works by entering the bloodstream via the intranasal pathway. It then crosses the blood-brain barrier and competitively binds to the same opioid receptors as opiates. Additionally, Narcan has a higher affinity for those opioid receptors and replaces the opiates causing the sedating effects.
The opioid family of medications compromises both legal and illegal substances. The most popular opioids include:
- Heroin,
- Fentanyl,
- Morphine,
- Vicodin,
- Percocet,
- Dilaudid,
- MS Contin,
- Methadone, and
- Codeine.
However, this is not a complete list. What’s more, street drugs are becoming increasingly more lethal because of the amount of fentanyl that may have been added.
It is essential to talk about the use of Narcan in our EP community given the exponential increase in opioid overdoses over time.
Opioids and their Effect on the Human Body
In recent years, it has dominated the news. Due to the drug’s strength, many other illicit narcotics are “cut” (or combined with) to heighten their euphoric effects.
Fentanyl is added to many narcotics like cocaine and heroin – as well as Percocet, Vicodin, and other painkillers – to increase their potency. Unaware that their drug or medication has been augmented, a user may take their regular dosage to feel high and wind up overdosing as a result of the effects of the fentanyl.
How Do Opioids Work on the Body?
Opioids, such as fentanyl and fentanyl combined drugs, can be injected intravenously, applied topically, taken orally, or inhaled. They attach to opioid receptors in the brain after crossing the blood-brain barrier. The effects of these opioids on the body are extensive, including:
- Relaxation,
- Euphoria,
- Pain relief,
- Sedation,
- Dizziness,
- Drowsiness,
- Confusion,
- Pupillary constriction,
- Slow heart rate, and
- Respiratory depression.
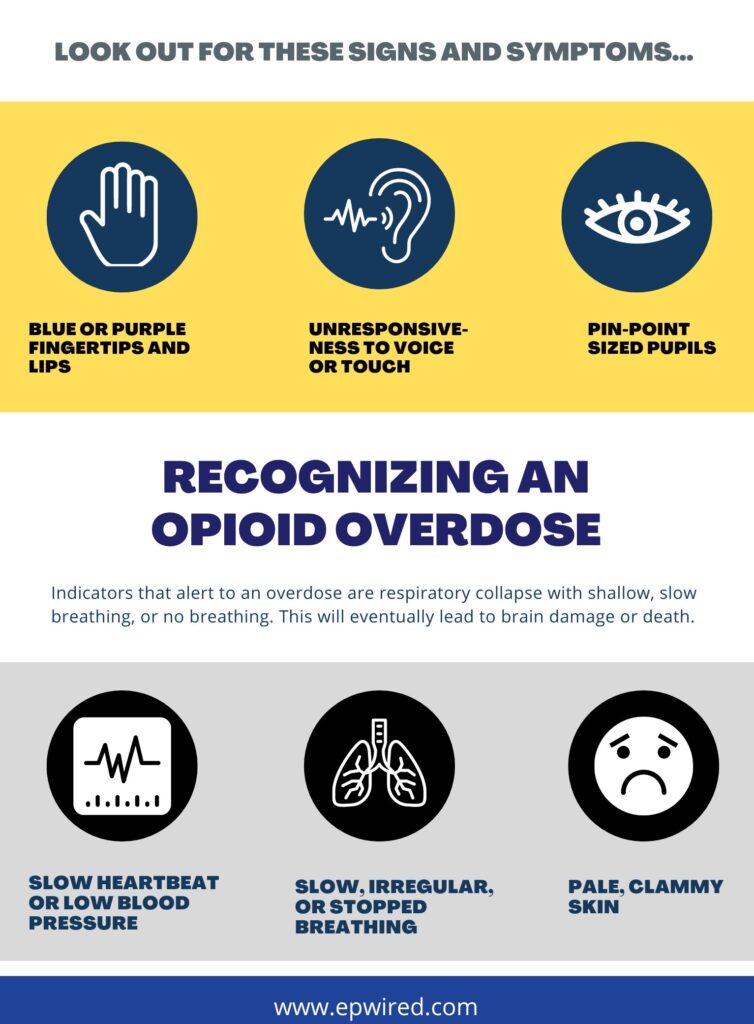
Recognizing an Opioid Overdose
An overdose can occur anywhere from 20 minutes to two hours after the use of substances. Signs of an overdose include the following:
Vitals
- Hypothermia (Low Body Temperature)
- Bradycardia (Low Heart Rate)
- Bradypnea (Low Respiratory Rate)
- Hypotension (Low Blood Pressure)
Mental Status
- Sedated, Comatose
Pupils
- Miosis (Constricted)
EP professionals and the Use of Narcan
In the security industry, some providers are sure to encounter illicit drug use by clients, friends, family, or guests. Any individual exhibiting the effects of an opioid overdose will need immediate attention and reversal.
Imagine this scenario: You are accompanying your client on a private yacht. Somebody on board starts to display signs of an overdose. There is no EMS unavailable, making you the initial medical provider.
That is where intranasal Narcan comes into play. As the EP agent, you may be the most qualified or only one prepared to assess and administer the life-saving treatment.
Who Else Should Carry Narcan?
The simple answer is anyone who may have to deal with someone at high risk for opioid overdose. Those who are at the highest risk are:
- People who use prescription opioids, especially those taking higher doses.
- Children are at greater risk of accidentally ingesting drugs.
- People who use opioids in combination with other sedating substances, such as benzodiazepines (Xanax, Ativan).
- Household members of people in possession of opioids (including prescription opioids).
- People with opioid dependence, in particular, follow reduced tolerance.
- People who inject opioids.
- People who use opioids suffer from medical conditions such as HIV, liver or lung disease, or suffer from depression.
Others who should consider access and use of Narcan are those living or working in areas that see high rates of opioid overdose.
Final Word on Narcan
Narcan does not have to be given to someone “high” or intoxicated on an opiate. Rather, someone eliciting signs and symptoms of an opiate overdose, as indicated by respiratory or circulatory depression, should be administered Narcan.
Other indicators that alert to the need for Narcan are signs of respiratory collapse with shallow, slow breathing, or no breathing. Additional signs include:
- Someone cool to the touch,
- Clammy with bradycardia, or
- Hypotension is an indicator of eminent circulatory collapse.
Furthermore, after the administration of Narcan, a reversal of overdose effects happens within a minute. What’s more, these effects can wear off, depending on the concentration of opiates in their bloodstream. And since the patient can have recurrent opioid overdose symptoms after the initial Narcan treatment, monitoring them following the use of Narcan is crucial.
Remember that giving Narcan in the field to someone severely intoxicated and not showing signs of respiratory or circulatory collapse is not advisable. In this instance, you may elicit severe opioid withdrawal in an opioid-dependent individual.
Disclaimer: If you decide that carrying Narcan is right for you, start by researching the laws of your community, any potential travel destinations, and your employer’s standard operating procedures.
For more information watch this video for a thorough overview of Narcan, and how its administered.
NARCAN® Nasal Spray 4mg Instructions for Use
Michael Guirguis, MD is Founder and Chief Medical Officer at Raven Medical Support Group. RMSG provides consulting, medical direction and oversight for private family offices and corporate executive protection programs that perform domestic and international duties. He is an Emergency Room Physician, and Reserve Sheriff Deputy for San Bernardino Sheriff Air Rescue. Dr. Guirguis has extensive experience in Pre-Hospital Care, Tactical Medicine, and EMS.







I would NOT recommend that an EP agent administer Narcan unless they were a trained Emergency Medical Technician (EMT), had official approved training in administering Narcan, and the client approves for the agent to have and use. it. The potential for liability here is overwhelming to say the least. Also on a yacht, the captain and crew should have some medical training and if Narcan is a consideration (drug usage), then I would recommend the same level of training for them.
Hi Jerry, I understand your concern over liability and thank you for your comment.
I would agree if an EP agent is carrying Narcan and they are working for a security entity, corporation, or private family office they should have approval from their organization to carry it. The organizations I oversee have access to Narcan and have the proper training and standing order to give it to those exhibiting opioid overdose symptoms.
Narcan is being handed in many states by pharmacists without a physician prescription, law enforcement officers, and is being given to family and friends of those who are at risk of OD.
California and many other states have standing order for Narcan use. You no longer need to be a medical provider or EMT to give this medication.
https://www.cdph.ca.gov/Programs/CCDPHP/sapb/CDPH%20Document%20Library/NSO_FAQ_Sept%202022_ADA.pdf
Here is the U.S. Surgeon General’s Advisory on Naloxone and Opioid Overdose.
https://www.hhs.gov/surgeongeneral/reports-and-publications/addiction-and-substance-misuse/advisory-on-naloxone/index.html
I knew this could be controversial so I added a disclaimer on the article. Hope that may have cleared up a few things.