In past editions of exclusive EP Wired interviews, we mainly discussed hard security-related skills. However, for this one, we talk to Michael Guirguis, MD, a consultant for corporate security and executive protection teams. We discuss Michael’s experience as an emergency medical director and how he sees medical oversight in our industry.
EP Wired: Before we arrive at the gist of your work and experience, can you share your story of getting into EP as a medical director?
Michael Guirguis: I grew up in southern California and have always been interested in being a police officer. I never imagined I would be a doctor, my first love was becoming a police officer or a pilot.
I played sports, football, and injured my back. Then, I had a herniated disc, so I could no longer play football and no longer do something physical like being a police officer.
So I ended up going to UCLA, which is a big college here in Los Angeles. During my rehab for my back, I saw many doctors, pain management specialists, and physical therapists. And medicine became an interest.
I ended up graduating and went to Harvard Medical School. During that time, a show ER was prominent in the United States. My personality is that I’m very attention-deficit, so I like to see something. I like to diagnose it. Then, I like to treat it and move on. I get more joy out of treating acute disease rather than treating chronic disease.
I left Boston and came back home to California and did my residency at Loma Linda trauma center. Then, I found out from a friend that Loma Linda had a working relationship with the sheriff’s department. So, during my last months of residency, I went to the Sheriff’s Academy. I worked for a sheriff’s department in Air Rescue as a flight physician. So, for the last 19 years, I’ve been flying as a flight doctor part-time, two days a week as a volunteer, with the sheriff’s department.
Then, I went to the sheriff’s academy. I’m able to carry a gun. I’m a sworn peace officer on the side. With the air rescue team and sheriff’s department, I’ve done time with air rescue, the dive team, the SWAT team, and search-and-rescue. Also, during my emergency medicine training, I really enjoyed all the pre-hospital and out-of-hospital work. So, that’s where I got involved in NASCAR, Indy Racing, racing, motor cross, a lot of these raves, concerts, and things that I enjoy doing.
I like to practice medicine outside of the hospital. It always has lots of challenges, and I like overcoming them. I’ve worked on some federal United States disaster medical assistant teams DMAT CA-2. I was the emergency medical director for the 911 system for San Bernardino County, Fire/EMS system for ten years. I’ve worked on sports medicine with some of our hockey teams, the LA Kings, minor league team, the Ontario Reign. I did that for five years.
So, how I got into executive protection was dumb luck. A friend I worked with knew a guy who knew a guy who was looking for a medical director for a private family office. So we went back and forth.
They did a background on me. I got hired about three years ago to run my current physician as medical director for this private family office, where I manage almost 100 personnel members who are being cross-trained as EMTs.
Our goal is to have them all trained in EMT basics. And we have many advanced providers, PJs, special forces guys that have medical training, 18 Delta, few naval special forces, many federal law enforcement personnel, people who have retired and come into the corporate protection, executive protection world.
So, it’s pretty much dumb luck. It’s almost perfect for me. Even in college, I was a bouncer in a nightclub for 2-3 years to help pay the bills. A lot of it was my wanting to do something to get my mind off medical school and college. And it was fun, and it paid well.
So, I’ve always had that law enforcement, protective mentality, trying to keep people safe, either on the medical side or the protection side. So, the corporate protection, EP world… I never thought I’d be doing something like this. It was just dumb luck that it happened. But it’s also like a perfect fit for me.
Some studies suggest that each year more than 18,000 Americans have a shockable cardiac arrest outside of a hospital that occurs in public with witnesses. How do you see this number spilling over into the executive protection industry? What role does an emergency medical director play in preventing principals’ deaths?
Like most things in the executive protection industry, we will be protecting clients, and common emergencies will happen, common in the community and with our clients.
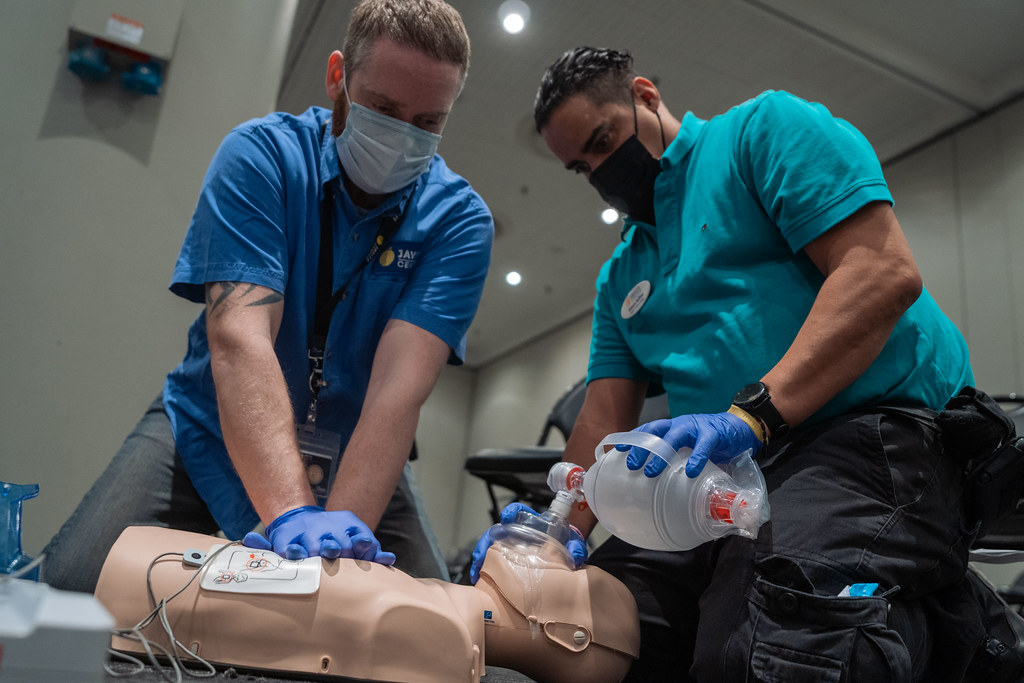
Depending on the client, maybe younger or older, they may have a higher risk for cardiac disease or stroke. Hence, we must be prepared to treat those. If our principal goes down and has no pulse, then we need to have an AED available and put it on them and see if it’s a shockable rhythm.
Like anything, the faster you can treat, the better their morbidity and mortality will be. And it’s been shown by multiple studies in terms of early recognition of cardiac arrest of MI (myocardial infarction), of a stroke being able to use CPR or an AED or get them to a hospital to decrease mortality and morbidity.
Also, early hemorrhage controls. Myriads of studies show trauma or injury where you can get better hemorrhage control will cause better outcomes.
The emergency medical director’s role is to oversee some of the advanced techniques we can use, the EMT basics, and the paramedic who can provide the care early, instead of just waiting for local EMS to arrive. Early treatment is always the standard. In fact, it’s described in some of these mantras, like the Golden Hour of Trauma. You want to get that patient to the trauma center within that first hour. You don’t want to spend a lot of time in the field.
There is a mantra: Time is Heart. In heart attacks, the faster you can get them to a hospital and cardiac cath them or do thrombolysis on them, the better outcome they will have. And the same applies to stroke. The faster you can get them to a stroke center and treat and reverse the stroke, if possible, the better they are going to do.
The Board of Executive Protection Professionals has started developing a process of a security standard for EP. Where do medical oversight and emergency medical directors fit within this broader framework of standards?
I was brought on to help with some basic medical training that each EP provider will need. So, nothing is set in stone. I’m just speaking based on what I think may happen. In the EP world right now, I think there will be a strong interest in emergency medical care.
Every EP company is not going to need a medical director. So, that’s not going to be the standard. But there is going to be some basic medical care, which will be part of the standard most likely. As I say this, it is all kind of my conjecture and what I think is going to happen.
So, personnel could be taking courses like TCCC or TECC, Stop the Bleed, and CPR/First Aid. I could see these as probably the maximum someone would have to know and the minimum I think any provider should have if they are going to be working in the EP field.
Being an emergency medical director will probably go onto some of the larger EP firms and EP teams that are seeing the wave of the future, where medical response integrated into their security is what clients want. Thus, you don’t really need a medical director for the average emergency medical responder who can do the basic skills of hemorrhage control via tourniquet or packing wounds, CPR, AED, basic BLS skills, and Heimlich maneuver.
But once you start getting more advanced, like putting in IVs, getting medication, doing airway protection, advanced skills, that’s where you start to need an EMT and a paramedic. And with that, you need medical oversight in the United States. That’s where an emergency medical director can help with the oversight, training, quality assurance, and quality improvement of what we do.
You have extensive experience providing medical care at mass gatherings, including large-venue music concerts and sporting events. Can you mention a few major challenges you have faced in the process? For example, what does communication look like with security professionals in such adverse events?
I think it’s a two-part question. Because, when I work mass gatherings, it’s not on the EP side. It’s for the event. But let’s say there will be a client with his security personnel. So, I think at that point, security personnel should have done their advance. If I’m working for the concert, then there should be a conversation with that team in advance. They will be able to know what exactly we are going to be able to provide and what we are not.
Obviously, we can have radios. If it’s a big client, it’s something we are going to want to work together with. Also, security personnel that goes to these big concerns are going to have to deal with people on drugs, on alcohol. With belligerent people. So that’s also a different dynamic.
There is some trauma in most of these concerts, raves, rock concerts, sporting events, and race car events. A lot of people don’t eat if it’s a hot day. It’s hypoglycemia and dehydration. A lot of these raves, which are some of the most medical treatment-intensive concerts, have lots of ODs, drugs, and a lot of hyperthermic ODs. A lot of these drugs will make your body really hot. They often need to be treated by sinking them in ice-cold water to get their body temperatures down, so they don’t fry their brain.
Many of these populations are younger but very sick due to the drugs they are using. So, the security personnel must be aware that there may be medical personnel onsite, but they will be swamped and may not be able to tend to their client.
One of the major things for docs or medics working these concerts is that they have to do a lot of treatment onsite. The reason is that when you bring in 60 to 100 thousand people in a small area with only a few surrounding hospitals, you can’t send every single sick person to the hospital. So, a lot of the treatment is done there: onsite.
You have to be aware of not inundating those hospitals. So, treatment basically happens there, and we call it Treat and Street. We treat them, and if they are stable, you can discharge them. If they are really sick, then those are the people who get sent off. Security always needs to have that in the back of their mind. If something terrible happens, like trauma, they may have to, on their own, evacuate, start treatment, and get to the hospital on their own because there may not be an ambulance or doctor available to see them in a timely fashion.
That’s something they have to be aware of when they go to those big events.
Due to their proximity to the protectees, many EPAs are also first responders when health crises arise, often with little experience. How then do you convince an executive protection company to hire an emergency medical director and the accompanying paramedics?
I don’t even need to convince them anymore. the market is going to do the talking. A lot of EP firms are starting to see that the medical is very important along with their security aspect. So they are already beginning to send their guys to TCCC, TECC, and many of these courses.
As these companies grow and start to add medical directors and advanced medics along with their security personnel, and they begin to offer these services to these clients, the companies that don’t follow suit will lose out on a lot of business.
Many of these EP firms are doing it because they know full well that they can offer these medical services and recoup the costs by charging more for the service. So, a client is willing to pay more to have security with a medical background. With a lot of these guys, we want them to be dual security and also cross-trained in medical. You don’t want just a medical guy there who you are paying, with no security background.
That client is going to be happy to pay an extra per hour to know that he has got a medical response, advanced medical available to them if something happens at the residence while traveling somewhere rurally, in a plane, over the Atlantic. In other words, for knowing that there is treatment available.
That being said, also post-COVID in the United States, there are a lot of delays in emergency care, 911. There is a shortage of medics. A lot of these older fire paramedics have retired because of COVID. They don’t want to get sick. Many people have left and have taken time off because of COVID. Therefore, that leads to longer scene time for local EMS.
Response times are delayed. ER staff are short. Nurses are working less, are stressed out and calling off, and moving to other departments where they are not exposed to COVID. Nurses aren’t available and are retiring. And even if you get to the hospital, you may have to sit on a gurney for a long time until you get treatment because there is no room or no nurses to take care of the patient.
That leads to EP firms needing to start seriously training their guys to provide medical care. They are going to be on the frontline as responders.
We all know that a location’s threat level will inform the scope of the provision of medical services. Suppose an EPA finds themselves in a Carribeans’ far-off area or remote locations in Africa or Australia. In that case, what should they have at hand, especially if the nearest medical facility is hard to reach within a reasonable timeframe?
Scenarios like this are where the emergency medical director and a strong security team with advanced medical background are needed. Before that trip, you have to conduct a medical advance.
You have got to know your client. You have to know where you are going. Are there local hospitals? What capabilities do they have? What’s their transport time if you are on a yacht off the Carribeans, twelve miles or five miles. How will you get that patient from your boat to the hospital on land? How long is that going to take? Do they have an EMS ambulance that will wait for you on the beach when you bring them in?
Is the EMS a volunteer fire department, or are they full-time? What capabilities do they have? Of course, you have to be ready for everything, like having:
- Advanced medical and trauma bags,
- Advanced airways if something happens, someone drowns on a boat, or someone cuts themselves,
- AED, a monitor, drugs if you are going to do CPR, you have a medic there who can give epinephrine. You have to be able to do that.
You can’t wait 30-45 minutes to move a patient from a yacht to a boat to get to shore. Additionally, you also have to have equipment for minor injuries. For example, you are not going to remove a client of his yacht, who may have sprained his wrist, maybe fractured it. You won’t take him to the local hospital. You may, but you may not.
Similarly, you may just assume it’s broken and splinted and then worry about going to the hospital now or later or reassess. So, you need equipment: splints, a soft tissue injury, a suture kit. But, on the other hand, maybe you got a minor cut that doesn’t need to go to the hospital.
If you have a paramedic or advanced medical on the boat, that can help. Medications for common illnesses, cough syrups, diarrhea medications, allergic reactions, pain medicine like Motrin Tylenol, maybe something more advanced if you have an emergency medical director, medication for allergic reactions, rashes, cremes, things like that.
With that in mind, you should also have telemedicine capabilities. So either you have it via your medical director, or you want to contract with a telemedicine provider. It’s like the Philips system we have. It has vitals and can upload information to a telemedicine provider. It has a monitor and can upload video chats.
But today, it can be done via an iPad or smartphone, and you can do telemedicine through your phone. It allows you to show the wound, infections, and other details. These telemedicine systems help you with some minor injuries, ailments, and things like that.
Also, you need antibiotics. Let’s say someone gets a cold, a cough, maybe pneumonia. You need to have antibiotics, antivirals, or antiparasitics if you are in a country with endemic parasitic disease. So you want to have those medications available, and that’s basically via a medical director.
And then have an evacuation plan. For example, if you are in the Carriebans, do you have a way to get the patient to the shore faster? Do you have a helicopter? Can your helicopter go from the shore to the United States if you are relatively close? What hospital would you go to? How do you set that up?
If you need more advanced transport, find a transport company that’s willing to provide medical transport and evacuation. Then make sure that the company is reliable. In other words, if something actually happened, they would be there.
What words of wisdom would you give to executive protection companies and solo practitioners regarding medical oversight and having an emergency medical director on-site?
As I stated earlier, the future of EP is just having highly skilled security personnel trained in your typical security hard and soft skills. But you also want them to be cross-trained in the hard skills of medical training, assessment, and treatment.
The industry is changing. EP teams will start to provide medical care because medicine and emergency medical services are beginning to become delayed in some of these communities where EMS and medical providers are pushing up their retirement and not working as much. And I think, sooner or later, providing medical care and basic medical care will become the standard of the EP industry.
On an everyday basis, in terms of having an emergency medical director onsite, I don’t think you need a medical director to be onsite. But you need security medical practitioners who have to practice, practice, practice those skills because they are very perishable. And because their job is mostly security, and rarely will they do medical, those skills are perishable. And I think, at least, by minimum, bi-weekly to monthly basis, they need to start to do training.
They don’t have to go to a formal class or get a formal certification, but they need to sit and be able to review one topic every few weeks and work with a friend or a colleague they are maybe working with that day. Just go over a case study, or how would you do an assessment for a patient found down on a property or someone who tripped and fell, hitting their head? What do you do? What are you looking for? The ABCs of trauma or basic medical assessment.
If a medical director doesn’t need to be onsite all the time, there may be scenarios where you want a physician traveling with you. For example, maybe the client is ill and wants someone there while they travel. Maybe the client is uncomfortable flying over the Atlantic on his private plane without any advanced medical on board. Perhaps you are going to a country where there is turmoil, or you are out in a rural area with no nearby hospitals.
If there is a high medical or threat assessment and a client is concerned, you may want your medical director or contracted physician to travel.
So, my big words of wisdom are to be a company at the forefront of the industry, to be a leader, and to have the majority of your personnel cross-trained in medical care.
I think they should all be cross-trained in basic medical care. But also have a select few with advanced skills so you can strategically place a paramedic or an EMT on each team. So there is always an advanced level provider on a security detail wherever that client goes.
Be that industry leader that offers those benefits instead of waiting until you are finally obligated to have to do it, and then you are trying to catch up.